Treatment access barriers are a significant obstacle to equitable healthcare access and a source of frustration for many patients. These barriers, including limited availability of services and excessive wait times, can severely compromise the quality and timely delivery of essential medical care. In this comprehensive guide, we delve into the complexities of these barriers, explore their far-reaching implications, and provide actionable solutions for improving access to treatment. We will explore the root causes of these barriers, analyze their impact on different patient populations, and offer practical strategies for improving healthcare systems. This article is structured as follows: First, we will explore the various types of treatment access barriers. Next, we will examine their impact on patient experience and overall health outcomes. Finally, we will present evidence-based solutions for eliminating these barriers and promoting equitable access to care.
Understanding Treatment Access Barriers
Defining Treatment Access Barriers
Treatment access barriers encompass a wide range of obstacles that prevent individuals from accessing necessary healthcare services. These impediments can range from logistical hurdles to systemic issues, hindering the pursuit of timely and effective medical interventions. These difficulties vary greatly depending on geographical location, socioeconomic status, and pre-existing health conditions. Moreover, a thorough understanding of these barriers requires acknowledging the interplay of individual-level factors and societal structures. Furthermore, access to quality healthcare is a fundamental human right; therefore, addressing these impediments is critical for fostering health equity and well-being.
Types of Treatment Access Barriers
One key factor impacting access is limited availability of services. This can manifest in a shortage of healthcare providers, inadequate infrastructure, or insufficient resources to meet the demands of a specific population. Another significant obstacle is the frustratingly long wait times often associated with accessing treatment. These delays can cause undue stress and anxiety for patients, leading to delayed diagnoses, compromised treatment outcomes, and potentially worsened health conditions. These significant issues often result in the need for substantial intervention to ensure smooth and timely care.
Impact of Limited Availability and Wait Times
Patient Experience
Limited availability and excessive wait times can have a profoundly negative impact on the patient experience. Patients often experience significant anxiety and stress related to the uncertainty of when or if they will receive needed care. Furthermore, these delays can lead to a decline in the patient’s overall health and well-being. This impact can be particularly acute for those with chronic conditions or urgent needs, who require prompt attention to prevent further complications. The cumulative effects of prolonged wait times can manifest in decreased adherence to treatment plans, increased healthcare costs, and diminished quality of life for individuals impacted by treatment access barriers.
Healthcare Outcomes
The repercussions of these barriers extend beyond the patient experience, impacting healthcare outcomes as well. Delayed diagnoses and treatments can lead to a worsening of conditions, necessitating more extensive and costly interventions. Additionally, there is an increased risk of medical errors and complications when patients are forced to wait excessive amounts of time for care.
Strategies for Addressing Treatment Access Barriers
Expanding Service Availability
One potential solution to address treatment access barriers is to expand the availability of healthcare services. This can be achieved through various strategies, such as increasing the number of healthcare providers, particularly in underserved areas. Furthermore, proactive investments in infrastructure, including facilities, equipment, and technology, can also significantly enhance accessibility. Also, improving transportation options and providing financial assistance programs are crucial steps to ensuring equitable access for vulnerable populations. Such improvements in resource allocation, in tandem with strategic community partnerships, are crucial for driving meaningful change.
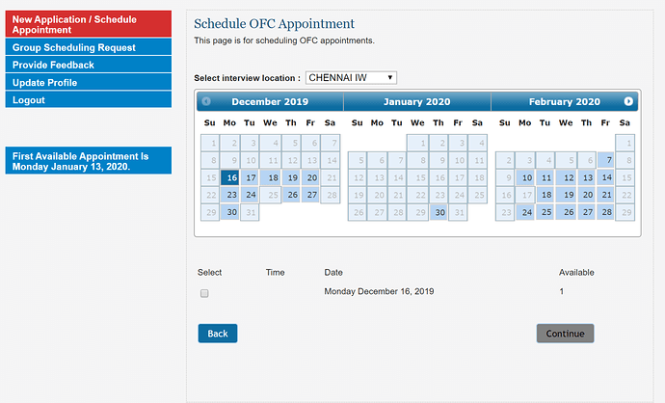
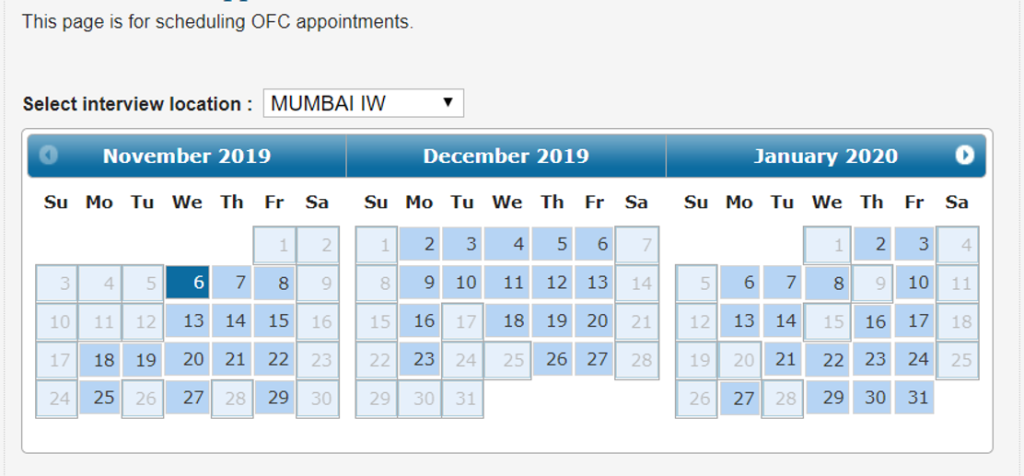
Streamlining Application Processes
Another critical aspect in alleviating these barriers lies in streamlining application processes for treatment. This can be accomplished by implementing efficient administrative procedures, using digital technologies, and providing clear communication channels. Making forms and procedures more user-friendly can significantly reduce the time and effort required for patients to access necessary treatments. These process improvements are critical to minimize administrative burdens and improve the patient experience.
Case Studies and Examples
Rural Healthcare
In rural communities, limited access to specialists is a pressing concern. Lack of transportation, extended distances, and the shortage of healthcare providers in rural areas often exacerbate these challenges. To address this problem, telehealth services can be leveraged to provide remote consultations and monitoring. Moreover, establishing mobile clinics and collaborative partnerships with nearby hospitals can offer more timely and effective treatment options.
Chronic Illness Management
Chronic illnesses require ongoing monitoring and management. Patients with such conditions frequently face significant hurdles accessing necessary resources, such as specialized care, support groups, and self-management education. Integrating telehealth tools, offering personalized care plans, and providing patient education programs can effectively mitigate these obstacles.
Data and Statistics
Prevalence of Barriers
Numerous reports highlight the prevalence of treatment access barriers in various demographics. Research consistently shows a correlation between socioeconomic status and the difficulty in accessing timely medical care. Further research is essential to identify the factors that contribute to these patterns and inform effective strategies to reduce disparities. More data on geographical location and the availability of services is needed. Moreover, more studies need to be done in the area of access disparities across racial and ethnic groups.
Impact on Health Outcomes
Data consistently shows a correlation between prolonged wait times and adverse health outcomes. By reducing wait times and improving treatment access, healthcare providers can significantly contribute to the long-term health and well-being of individuals and communities.
In conclusion, overcoming treatment access barriers is crucial for equitable healthcare access. Improving communication, expanding telehealth options, and streamlining application processes are just a few of the steps that can be taken to enhance the treatment experience for all. By actively addressing these barriers, healthcare providers can ensure that patients receive the care they need, when they need it. To learn more about specific solutions and resources available, visit our website at [website address].